What is Palliative Care?
If you have been told your cancer cannot be cured or that you have a life limiting illness, this would often called a palliative condition. Palliative care does not mean you won’t be offered any treatment or care. Palliative care is based on the needs of the patient, not on how long a patient might live. Palliative care is for people of any age and at any stage in a serious illness, and it can be provided along with curative treatment. Palliative care is provided by many health professionals such as your cancer doctor or nurse, GP or District Nurse or for more complex needs by a specially trained team of specialist palliative care doctors, nurses and other professionals.
The healthcare professionals caring for you will offer to talk to you (and anyone else you would like to be involved) about what this means for you. Ideally these conversations happen when you are well, so that should you become unwell your care team is aware of any wishes you may have, and your individual support needs. A key aim of palliative care is to maximise your quality of life, by treating and relieving symptoms and side effects of your illness. This is combined with the offer of support for you, your family, friends and carers, both in practical terms and emotionally.
How to Access Palliative Care Support
If you or a loved one is facing a serious illness, you may benefit from palliative care. You can have palliative care at any point in your illness. Speak to your GP, Hospital doctor or Nurse for more support.
For more specific information about Palliative care services at South Tyneside and Sunderland including St Benedicts Hospice please click here.
Treatments
Palliative treatment
The aim of receiving palliative treatment is to improve your quality of life and relieve symptoms. It can be used at any stage of an illness if there are troubling symptoms, such as pain or sickness. In advanced cancer, palliative treatment might help someone to live longer and more comfortably, even if they cannot be cured.
Palliative treatment is not just about medicines to control symptoms - such as painkillers and anti sickness drugs. Cancer treatments can also reduce or get rid of symptoms. For example, they can help to reduce pain by shrinking a tumour and reducing pressure on nerves or surrounding tissues. Treatments used in this way include please click on links below:
• chemotherapy
• radiotherapy
• hormone therapy
• targeted cancer drugs
• surgery
• radiofrequency ablation, which uses heat to kill cancer cells
• Cryotherapy, which uses extreme cold to destroy cancer cells.
Symptom Management
Relieves Suffering from Symptoms and Stress
The goal of palliative care is to relieve suffering and provide the best possible quality of life for patients and their families. Symptoms may include pain, depression, shortness of breath, fatigue, constipation, nausea, loss of appetite, difficulty sleeping, and anxiety. The team will help you gain the strength to carry on with daily life. In short, palliative care will help improve your quality of life.
Please try not to be worried about a referral to palliative care, it has been shown that patients with a serious illness who received palliative care lived longer than those who did not receive this care, and our focus is that you have our support to improve your quality of life at this time.
Videos
Advance Care Planning
When you are faced with a life limiting illness it can be helpful to consider what is important to you and how you would like to be cared for. It is then also helpful to share these thoughts and wishes with your family, carers and health professionals, to ensure that we can support you to try and achieve these.
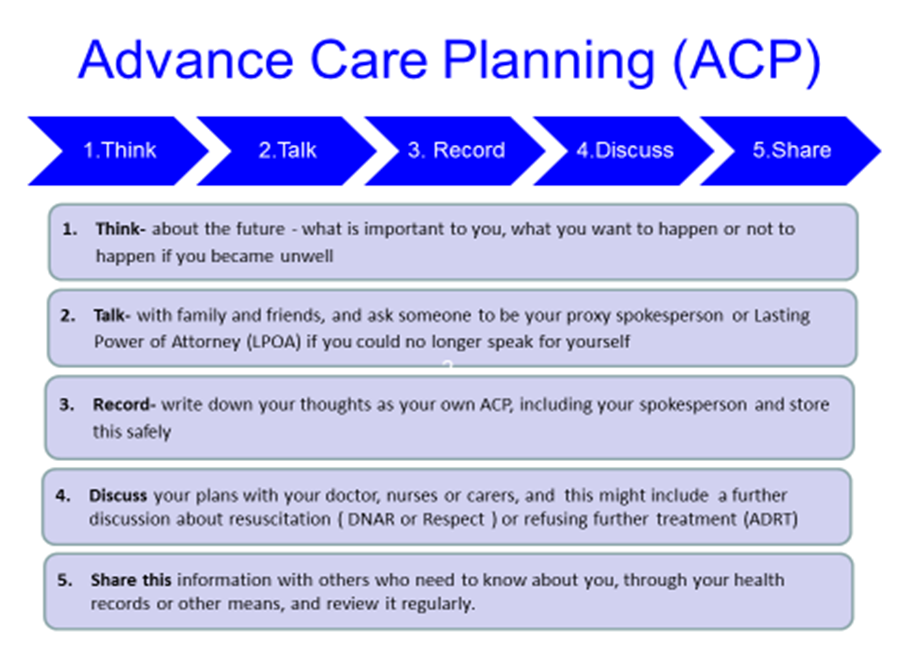
Advance Care Planning is a way to think ahead, to describe what’s important to you and to ensure other people know what your wishes are for the future. It’s about helping you to live well right to the end of your life.
When thinking about your advance care plan you might want to think about where you would like to be cared for in the last days of your life. Would you want to be in your own home, admitted to hospital or a Nursing home or Hospice? Would you want to come to hospital for treatments such as antibiotics and fluids or prioritise staying at home with loved ones? Do you have any thoughts about who you would want to be with you during this time, or who you would prefer didn’t visit! Thinking ahead, discussing with others and writing things down means that your wishes are known and respected, and you are more likely to receive the kind of care you want.
Please watch this video which explains visually what Advance Care Planning is helpful for.
Advance care Planning is a very simple process – it’s just 5 simple steps.